Member Spotlight
Brief profiles that highlight our members achievements and their contributions to our communities.

April 3, 2024
Tell us a bit about your work in planetary health.
I’m currently involved in a project to survey members of IPAC on their understanding of the Canadian Environmental Protection Act (1999) and the recently passed Bill S-5, known as the Strengthening Environmental Protection for a Healthier Canada Act (2023). Bill S-5 introduces the notion that Canadians have the right to a healthy environment, and I’m currently surveying IPAC members to better understand their perspectives on what this means within the context of Indigenous communities, who are disproportionately impacted by the changing environment.
What drew you to working on the Bill S-5 survey?
Throughout my academic and professional career, I’ve sought opportunities to work with and on behalf of Indigenous communities. Given that the Indigenous people of Canada have already begun to feel the effects of our changing climate, I’m hoping that the research I’m conducting will contribute to building a healthier and more sustainable environment for future generations.
If you could ask your fellow IPAC members to do one thing for planetary health, what would it be?
I believe that education is an essential first step in improving the health of our planet – it’s challenging to make a meaningful contribution to improving the state of our environment without understanding our local, region, and national policies on environmental protection. To that end, I would encourage members to join the Citizens Climate Lobby, an international grassroots environmental group that trains and supports volunteers to build relationships with their elected representatives in order to influence climate policy.
January 11, 2023
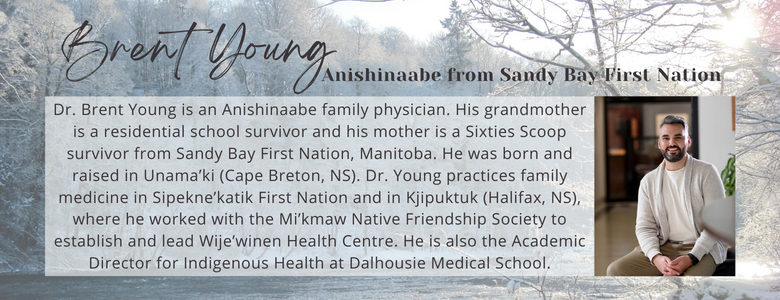
What made you decide to pursue family medicine?
I decided to pursue family medicine because of the versatility and flexibility it offers. I knew it would allow me to work in a variety of community settings with a broad scope of practice. I have been particularly happy with how it has allowed me to practice on- and off-reserve. Despite some of the challenges seen within family medicine, it is one of few specialties that allows for rich longitudinal relationships with patients and their families. A strong relationship with a family physician is the foundation for restoring trust between Indigenous people and the healthcare system.
How would you describe your work with the Indigenous Community?
I wear a number of hats in my work with the Indigenous community. In my practice, I provide primary care services to two communities: One that is predominantly Mi’kmaw and living on-reserve, and one that is composed of diverse First Nations, Inuit, and Métis individuals living in the urban setting. Each of these communities has distinct values and needs. I also serve as the founding Clinical Lead for Wije’winen Health Centre. I established this clinic among a wider umbrella of services offered by the Mi’kmaw Native Friendship Society. It has been amazing to be able to refer patients to such a wide array of programs and services that are culturally safe and relevant. Wije’winen Health Centre is a huge source of pride for me and my community. In my separate role as Academic Director for Indigenous Health at Dalhousie Medical School, I helped develop a new Indigenous Admissions Pathway to undergraduate medical education. Through a new holistic review process, this pathway will significantly increase the number of Indigenous people admitted to the medical school. The first cohort is expected to enter in August 2023. I am also involved in leadership roles with the Doctors Nova Scotia Section for Indigenous Health, the National Consortium for Indigenous Medical Education, and the College of Family Physicians of Canada Indigenous Health Committee.
October 12, 2022
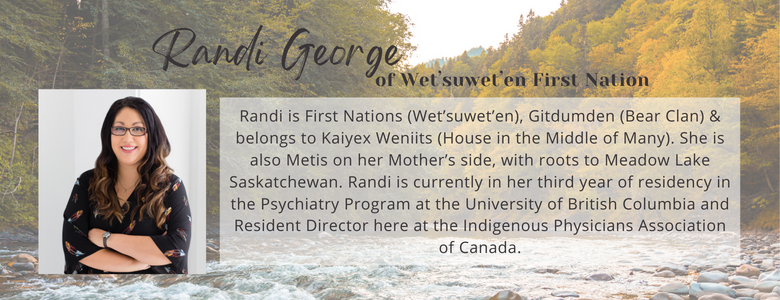
What led you to choose Psychiatry as a Specialty?
My life journey led me to Psychiatry. Born & raised on Reserve, I witnessed & experienced the impacts of Colonization, including trauma. When I was 5 years old, I lost my cousin to suicide just months before she graduated high school. I didn’t know much about mental health then, but I knew that I didn’t want her death to be in vain. After University, I worked at a Medical Clinic that served the Indigenous, disadvantaged, & marginalized downtown population. Again, I saw the impacts of trauma on our People, in the form of mental health & substance use struggles. In Medical School, I connected with my Psychiatry rotation because I was finally able to focus on the aspect of medicine I am most passionate about, namely the impacts of childhood & intergenerational trauma. The interview style of listening to a patient’s life story, understanding how their past & familial experiences impact them today, reminded me of Indigenous ways of teaching & learning – through storytelling. The Bio-Psycho-Social approach reminded me of our Medicine Wheel, where we not only consider one’s physical health, but also their mental, emotional, & spiritual wellness for complete health & healing. I feel like being a Specialist on the impacts of trauma also helps me with my education & advocacy work.
How would you describe your work with the Indigenous Community?
I was fortunate to be raised on my Father’s Traditional Territory, learning my culture, traditions, & history. At just 9 years old though, we moved off reserve to pursue further education & opportunities. This was the first time I faced the realities of racism. I was bullied & discriminated against to the point I hated school & was failing nearly everything. Then, I was told I couldn’t do & wouldn’t be anything so I decided to prove them wrong. I became a straight A student to prove I was worth something in society. To avoid further discrimination, I disconnected from my culture & identity for many years. It wasn’t until my work at the Native Health Clinic that I finally re-connected with my Indigenous identity & healed through that pain. I decided I wanted to pursue medicine with the goal of healing our traumas, AND working in education & advocacy with regards to the issues faced by our People & Communities. Through medical school & Residency, I have been heavily involved in this work, presenting to medical students, residents, & physicians across Canada on our history of colonization & how that impacts our experiences in medicine as Indigenous Peoples, whether as patients or practitioners. I advocate for equity in both training & treating our People in the medical system.
March 16, 2022
Why did you choose rural/remote family medicine?
By clerkship, I knew that I preferred working in smaller community hospitals and, because of this, elected to complete several core rotations and electives in rural and remote settings. I found that the clinical and community experiences in these places were simply unparalleled. Highlights include time spent in Moose Factory, ON and Iqaluit, NU. I was drawn to remote medicine, in particular, because of the breadth of practice, the adaptable and adventurous nature of colleagues and community members, and the strength of patient-provider relationships. I enjoyed the advocacy that came with working in resource-limited settings, and the satisfaction that came with making a difference, however small, in places where there exists a great need. As a novelty-driven individual with diverse interests, I appreciated that I was continuously learning from new clinical and extracurricular experiences. Living and working in an austere environment perpetually pushes individuals to build strength and resolve in themselves, and in this way helps us to reach our full potential not only as clinicians, but as people – this is something I aspire to achieve!
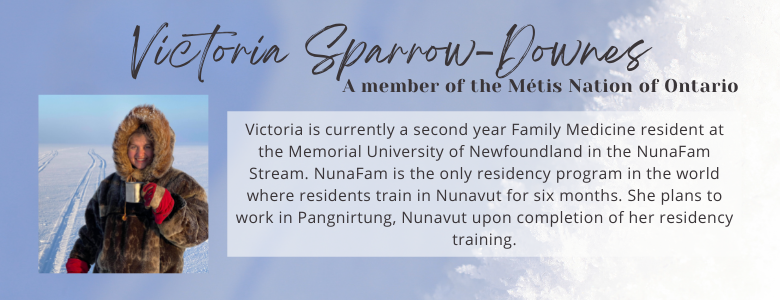
What journey led you to NunaFam?
I completed medical school at uOttawa, which has a longstanding healthcare relationship with Nunavut. In my first year of medical school, I participated in a clinical placement at Akausivik Inuit Family Health Team – an Inuit-specific family health clinic located in Ottawa, ON – and the only clinic of its kind in the world. I very much enjoyed the work there, and this was the spark that piqued my interest in exploring Nunavut. After finishing the placement, I began reaching out to physicians at Qikiqtani General Hospital, and eventually connected with the Director of Medical Education, Dr. Patrick Foucault, who I now consider one of my mentors. Dr. Foucault arranged for me to travel to Nunavut for a clinical placement in my second year of medical school, which proved to be a transformative event in my life. During this placement, I worked with generalist physicians to provide care in person and via Telehealth on a variety of services, including: emergency department, family medicine clinic, fracture clinic, general practice anesthesia, hospitalist, obstetrics, surgical assist, TA clinic, and TB clinic. I returned to Nunavut for an elective during my 4th year of medical school and was reminded of the rich and varied experiences and the joy to be had in this remarkable place, which solidified NunaFam as a residency choice! I am now nearing the end of nine consecutive months here, and feel much gratitude for having had this completely life-changing experience and adventure!